In this blog I talk about research into adverse childhood experiences, or “ACEs”, a term that is gaining in popularity. I did a quick search for “adverse childhood experiences” on PubMed, and the number of results per year speaks for itself. But what are ACEs, and how do they link with mental health and self-harm in particular? I am currently researching this topic at the University of Bristol, exploring the biological mechanisms that may explain the links between ACEs and self-harm. We don’t have published results as yet, so this blog is a discussion of the subject area.
Figure: Number of publications with “adverse childhood experiences” in the title or abstract by year.
NB: The study in 1970 mentioned adverse childhood experiences in a clinical sample of individuals with depression
Source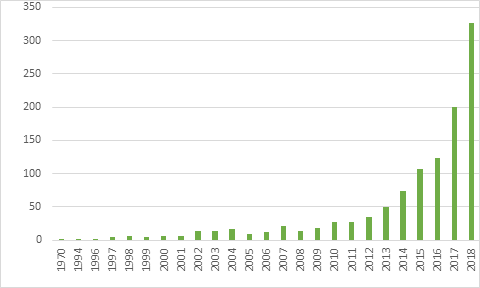
Adverse childhood experiences
Adverse childhood experiences, or “ACEs” is a term whose use was popularised following a study in the 1990’s. American researchers Vincent Fellitti and Shanta Dube asked adults enrolling in a health insurance scheme in Kaiser Permanente (USA) to complete a questionnaire indicating whether or not they had experienced any of a list of childhood adversities. Strikingly, they found that the more different ACEs people had experienced, the higher the risk of a range of negative physical and mental health outcomes – including suicide attempt (Dube et al., 2001; Felitti et al., 1998). Dube followed this work by examining ACEs in four birth cohorts with a total of over 17,000 individuals. She showed that for each additional ACE, the risk of a history of suicide attempt increased by 50-70% (Dube, Felitti, Dong, Giles, & Anda, 2003).
ACEs are indicators of child maltreatment and household dysfunction. They commonly include physical, sexual and emotional abuse, neglect, witnessing domestic violence, parent criminality, parental separation or divorce and parent serious mental health problems or suicide attempt. Other ACEs have also been used, including low socioeconomic status or poverty, and other experiences of victimisation such as bullying.
It is important to be aware that ACEs are common: the majority of people experience at least one childhood adversity. In a recent systematic review and meta-analysis, 57% of people had experienced at least one type of ACE and 13% at least four (Hughes et al., 2017). Research has consistently shown that those who experience multiple types of ACEs are at highest risk of negative outcomes. Yet the mechanisms through which these associations might operate are not well understood. This includes not knowing whether ACEs have a relatively direct link to negative outcomes or whether experiencing multiple ACEs indicates a high likelihood of other traits which are themselves associated with poor outcomes.
As a hypothetical example, let’s say that impulsivity is linked with ACEs. Children of impulsive parents may be more likely to experience ACEs themselves, and to be impulsive themselves because of their parents’ traits. Impulsivity as a personality trait is also linked to a higher likelihood of involvement in accidents, unplanned pregnancy, self-harm and substance use. Therefore, an association we observe between ACEs and self-harm may not be directly due to ACEs, but to impulsivity.
One of the outcomes that ACEs have consistently been linked with is deliberate self-harm, a term that includes self-harm with no suicidal intent through to suicide attempt or suicide (Björkenstam, Kosidou, & Björkenstam, 2017; Björkenstam, Kosidou, & Björkenstam, 2016; Hawton & James, 2005; Hawton, Saunders, & O’Connor, 2012). Self-harm is most prevalent in late adolescence and early adulthood: around one in five young people will self-harm at some point. The act of self-harm can cause both physical and psychological damage to an individual, and causes distress for those who are close to the adolescent (Björkenstam et al., 2016; Hawton et al., 2012). A history of self-harm is common in those who tragically die by suicide, although suicide is uncommon in adolescence even amongst those who self-harm (Geulayov et al., 2018; Hawton et al., 2012).
Preventing ACEs from occurring at all is perhaps unfeasible and a major undertaking that will require joined up working by a wide range of service providers. As with many factors, ACEs occur in intergenerational cycles, and some of the negative outcomes associated with ACEs increase the likelihood of the next generation experiencing ACEs themselves. Personally, I am aware of two areas that have begun to tackle this challenge: Wales and Bristol. In Bristol, the City Council, NHS, police and voluntary sector partners are collaborating as part of the “One City” initiative by the City Office. The One City plan sets out shared community goals for the city in the next 30 years. Mental health is an important theme, including reducing ACEs and suicide prevention. There are ambitions to make Bristol an “ACE Aware City”, training public service staff by 2020 and having all parents aware of the future impact of ACEs on health and wellbeing by 2025. These efforts are laudable and have great potential benefits but are unlikely to have immediate impact on rates of self-harm: there is a need for a clearer understanding of what aspect of ACEs lead to increased risk of deliberate self-harm. If we can pick apart the mechanisms that explain this association this could lead to i) identifying those at risk of self-harm, ii) potential treatment or preventative approaches, and iii) ultimately reducing the number of young people who self-harm.
The potential of using measures of ACEs in order to target treatment or as a screening tool has also been criticised- see this blog by Edwards and Finkelhor (2018). Others suggest ACEs are an ‘indicator of risk’ rather than a risk factor for poor mental health – Mind The Brain blog.
Mechanisms linking ACEs and self-harm
Whether the mechanisms that link ACEs and self-harm are entirely psychological or have biological underpinnings is not known – as with most long-term health problems it is likely to be as well as interactions between the two. Psychological mechanisms have been shown to mediate the association between some types of ACEs and self-harm without suicidal intent (e.g. Maniglio, 2011). A recent longitudinal study that focussed on psychopathology as a potential mechanism found different mediators of the association between ACEs and self-harm depending on the type of ACE. For children who experienced neglect, depressive and anxiety symptoms were a mediator, and for those who experienced physical or psychological abuse, the mediator was impulsivity and problems with attention (Paul & Ortin, 2019). Self-harm in this study was measured by parent report when children were nine years old.
The work I am currently doing at the University of Bristol focusses on potential biological mechanisms linking early life adversity and later self-harm. I work on a project funded by the MRC (Principal investigator Dr Becky Mars) exploring three of these potential mechanisms in more detail -look out for our findings in the next few years.
Because ACEs are also associated with poor physical health later in life, some research has suggested that these experiences become “biologically embedded”- where experiences lead to changes in a person’s development and biology (Hertzman, 1999). There are several plausible explanations for how ACEs become biologically embedded – for more detail see Berens, Jensen, and Nelson (2017). Let’s think about one instance of an ACE, for example witnessing domestic violence. When a child sees the violent event, their ‘fight or flight’ response or hypothalamic-pituitary-adrenal (HPA) axis is activated. This is a neuroendocrine stress response, meaning that both neurological and endocrine (hormonal) pathways are activated. This sets off a cascade of biological events, including release of cortisol and activation of the immune system. Whilst the single occurrence of an ACE may not lead to prolonged biological changes, if the stress-response system is repeatedly activated this could cause lasting changes (biological embedding). This could lead to: altered connections between neural pathways; dysregulation of the HPA axis; resistance to the effects of cortisol; dysregulation of the immune system; and epigenetic changes, whereby the molecules responsible for scaffolding our DNA change, leading to altered gene activity without editing the DNA code (for an accessible introduction to epigenetics see this YouTube 3 minute film) (Berens et al., 2017). All of these pathways could produce lasting changes in health and behaviour.
Inflammation is a good candidate mechanism for our exploration of the ACE-self-harm association, not least because it is something that can be measured with relative ease in people of all ages and could be a useful biomarker to indicate risk of self-harm. The immune theory of psychiatric disease (Beumer et al., 2012) draws attention to the wide-ranging physiological impacts of activation of the immune system. Several of the molecules released in the inflammatory response (‘inflammatory markers’) can cross the blood-brain barrier, which in turn can affect neural transmission and pathways, impacting on cognitions and behaviour. Studies have shown associations between ACEs and levels of inflammatory markers (Baumeister, Akhtar, Ciufolini, Pariante, & Mondelli, 2016; Coelho, Viola, Walss‐Bass, Brietzke, & Grassi‐Oliveira, 2014). Similarly, levels of inflammatory markers have also been associated with self-harm (Kim, Szigethy, Melhem, Saghafi, & Brent, 2014) although for both ACEs and self-harm there have also been studies that have not found evidence of an association.
Research methods to understand the association between ACEs and self-harm
I am currently using a couple of different research methods to try and untangle the association between ACEs, immune system activation and self-harm. In the first, a prospective cohort study, we are exploring whether levels of inflammatory markers (indicators of immune system activation) measured in a blood sample at age nine explain part of the relationship between the number of different ACEs a child has experienced before their 9th birthday, and whether they report any history of self-harm at the age of 16. Longitudinal birth cohorts are an excellent tool for examining models that try to explain the mechanisms by which two things are related, as we can clearly define when we choose measures of ACEs, inflammation and self-harm so that we can be sure that they do not overlap in time.
To complement this, we are also using Mendelian Randomisation (for an overview of Mendelian Randomisation see this 2 minute YouTube film) (Davey Smith & Hemani, 2014). This is a technique that aims to remove the influence of any confounding environmental factors. For example, BMI is associated with both inflammation and with self-harm, and so any association you observe between inflammation and self-harm could actually be confounded by BMI. MR gets around this by using genetic data. First you identify common genetic variants that are associated with measures of inflammatory markers. You then use these genetic variants to see if people who are genetically predisposed to higher levels of inflammatory markers are at a higher risk of self-harm than those who do not have these genetic variants. If we do find an association, it would suggest that inflammation itself may somehow contribute to the causes of self-harm; as your genes are fixed from conception, it is unlikely that they are affected by life experiences that might confound this association. Although gene expression may be altered by epigenetic changes, MR overcomes these issues of reverse causation (e.g. self-harm altering the epigenome and thus expression of genes related to inflammation). In order to conduct studies like this, very large sample sizes with genetic data are needed, and we make the most of resources such as the UK Biobank, the ALSPAC cohort and international genetics consortiums, who gather genetic data on tens of thousands of individuals.
We plan to go on to explore two other potential mechanisms that might explain the association between ACEs and self-harm. One is early or late puberty relative to the peer group, the other being DNA methylation – which is a specific type of epigenetic modification. Alongside this, research focussing on psychological mechanisms and other potential biological pathways is needed.
ACEs are not something that are measured in a standardised manner. They represent a variety of childhood environmental circumstances and relationships that might have different impacts depending on the nature of the ACE and on individual resilience to the effects of ACEs. Research that focusses on unpicking the reasons why ACEs predict negative health outcomes throughout life, and why some people do better than expected given exposure to ACEs might also help us to understand the best ways to promote resilience and prevent later mental health challenges for those who experience early adversity.
References
Baumeister, D., Akhtar, R., Ciufolini, S., Pariante, C. M., & Mondelli, V. (2016). Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Molecular psychiatry, 21(5), 642.
Berens, A. E., Jensen, S. K., & Nelson, C. A. (2017). Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC medicine, 15(1), 135.
Beumer, W., Gibney, S. M., Drexhage, R. C., Pont‐Lezica, L., Doorduin, J., Klein, H. C., et al. (2012). The immune theory of psychiatric diseases: a key role for activated microglia and circulating monocytes. Journal of leukocyte biology, 92(5), 959-975.
Björkenstam, C., Kosidou, K., & Björkenstam, E. (2017). Childhood adversity and risk of suicide: cohort study of 548 721 adolescents and young adults in Sweden. bmj, 357, j1334.
Björkenstam, E., Kosidou, K., & Björkenstam, C. (2016). Childhood household dysfunction and risk of self-harm: a cohort study of 107 518 young adults in Stockholm County. International journal of epidemiology, 45(2), 501-511.
Coelho, R., Viola, T., Walss‐Bass, C., Brietzke, E., & Grassi‐Oliveira, R. (2014). Childhood maltreatment and inflammatory markers: a systematic review. Acta Psychiatrica Scandinavica, 129(3), 180-192.
Davey Smith, G., & Hemani, G. (2014). Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Human molecular genetics, 23(R1), R89-R98.
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. Jama, 286(24), 3089-3096.
Dube, S. R., Felitti, V. J., Dong, M., Giles, W. H., & Anda, R. F. (2003). The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Preventive Medicine, 37(3), 268-277.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine, 14(4), 245-258.
Finkelhor, D. (2018). Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abuse & Neglect, 85, 174-179.
Geulayov, G., Casey, D., McDonald, K. C., Foster, P., Pritchard, K., Wells, C., et al. (2018). Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): a retrospective study. The Lancet Psychiatry, 5(2), 167-174.
Hawton, K., & James, A. (2005). Suicide and deliberate self harm in young people. BMJ, 330(7496), 891-894.
Hawton, K., Saunders, K. E., & O’Connor, R. C. (2012). Self-harm and suicide in adolescents. The Lancet, 379(9834), 2373-2382.
HERTZMAN, C. (1999). The Biological Embedding of Early Experience and Its Effects on Health in Adulthood. Annals of the New York Academy of Sciences, 896(1), 85-95.
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., et al. (2017). The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health, 2(8), e356-e366.
Kim, J.-W., Szigethy, E. M., Melhem, N. M., Saghafi, E. M., & Brent, D. A. (2014). Inflammatory markers and the pathogenesis of pediatric depression and suicide: a systematic review of the literature. The Journal of clinical psychiatry, 75(11), 1242-1253.
Maniglio, R. (2011). The role of child sexual abuse in the etiology of suicide and non-suicidal self-injury. Acta Psychiatr Scand, 124(1), 30-41.
Paul, E., & Ortin, A. (2019). Psychopathological mechanisms of early neglect and abuse on suicidal ideation and self-harm in middle childhood. [journal article]. European Child & Adolescent Psychiatry.



Discussion
Thank you for the interesting blog and very relevant research topic. In our CAMHS, ACEs are formulated as “traumatic experiences” and the clinical consequences of repeated exposure to ACEs as PTSD. Unsurprisingly, we have very long waiting lists for trauma treatment and the vast majority indeed present with self-harm. In your view, what is the relationship between ACE and trauma? Do you see them as interchangeable terms?
Best wishes
Fernando